Established procedures
In accordance with the SMOB guidelines, established surgical procedures are categorised into two distinct groups: basic procedures, which may be performed in all centres, and complex procedures, which may only be carried out in SMOB-recognised reference centres with a simultaneous HSM service mandate.
Basic procedures
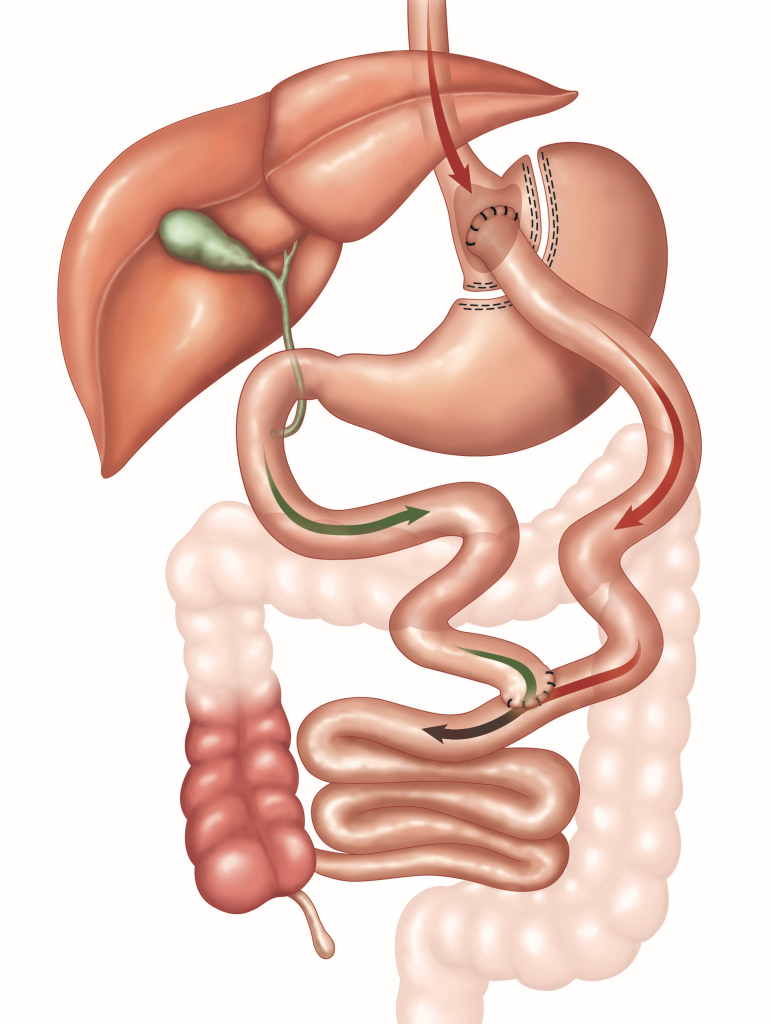
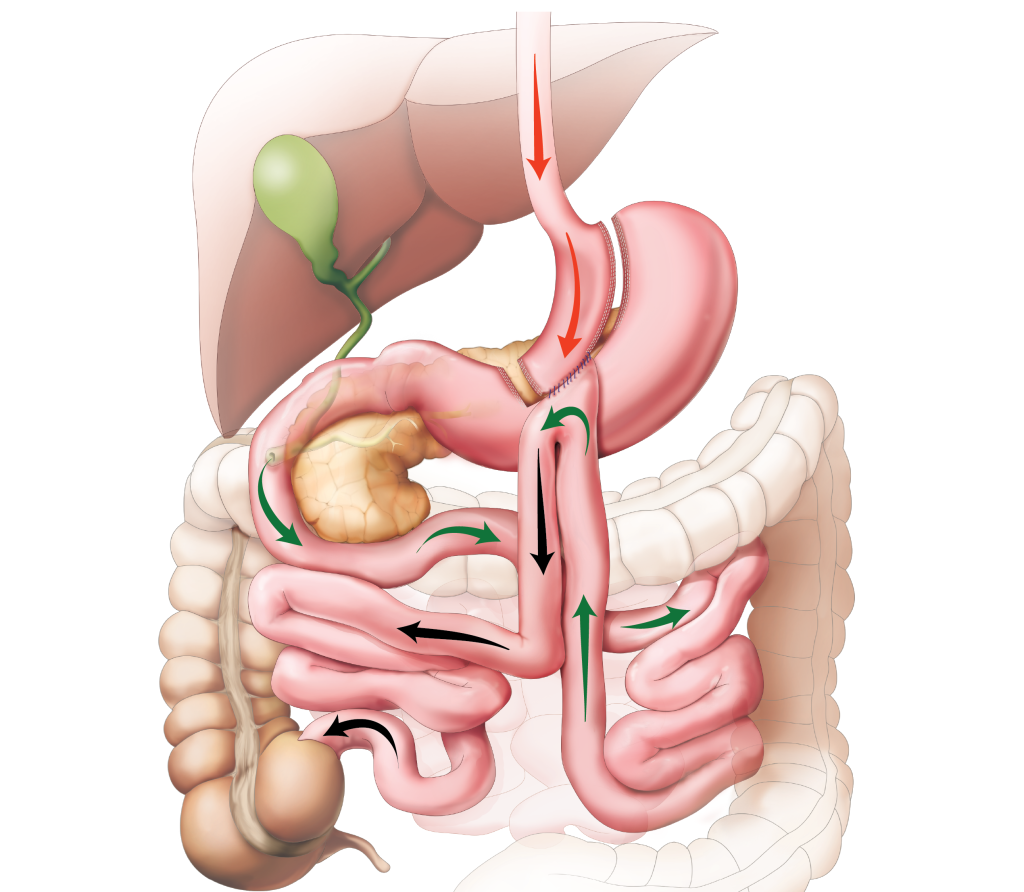
Roux-en-Y gastric bypass
In a Roux-en-Y gastric bypass (RYGB), the food mass is separated from the digestive juices in the upper gastrointestinal tract by creating a small gastric pouch directly below the oesophagogastric junction. This remaining stomach, which is no longer used for the passage of food, remains in situ. The jejunum is divided 50-70 cm aborally from the duodenojejunal flexure (Treitz’s flexure) and anastomosed to the gastric pouch (alimentary limb). About 150 cm below the gastrojejunostomy, the remaining part of the jejunum is connected laterally to the alimentary limb of the jejunum. This type of operation is also used in oncological stomach surgery and is reversible, although it is only necessary in very rare cases, for example if there are complications.
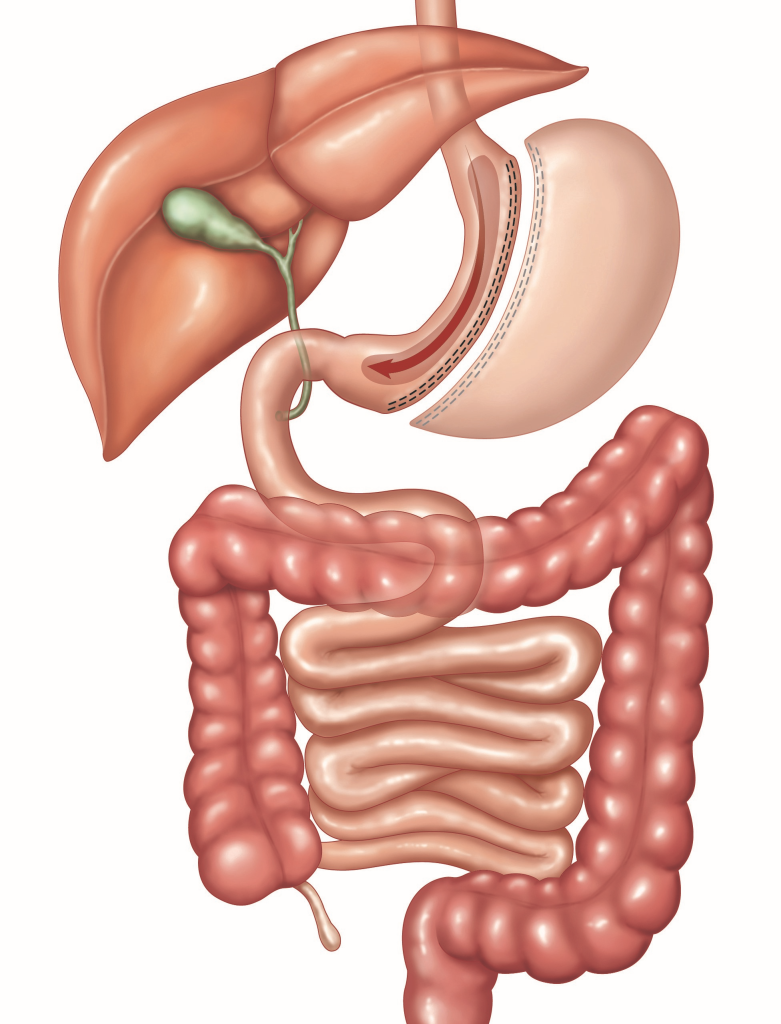
Sleeve gastrectomy
A sleeve gastrectomy preserves the anatomical food passage and the mixing of food mass with digestive juices. This surgical method is simpler than RYGB, with approximately 90% of the stomach volume being removed along the greater curvature, leaving a tubular residual stomach with a capacity of approximately 80-100 ml.
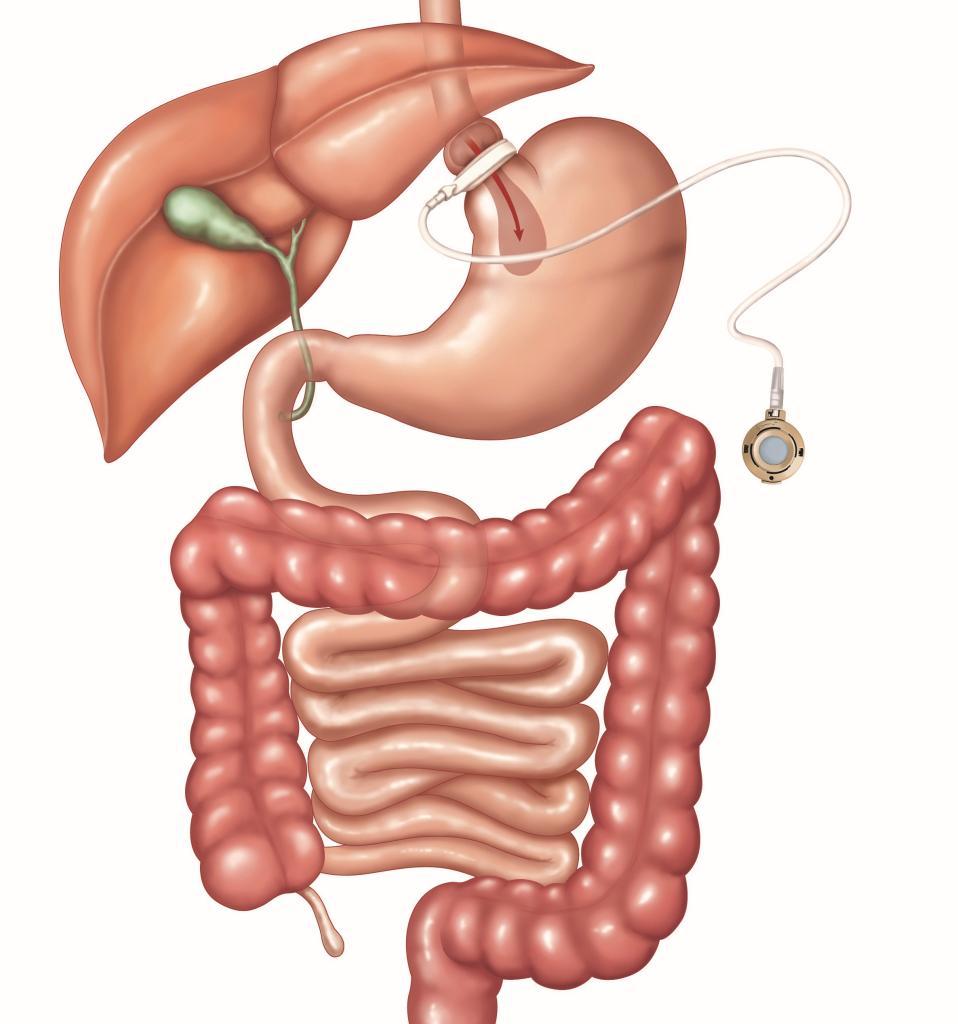
Gastric band
Adjustable gastric band surgery was the dominant bariatric surgical procedure between the mid-1990s and mid-2000s. However, due to unsatisfactory long-term results, this procedure is now rarely performed (approximately 1.3% of all bariatric procedures in Switzerland in 2022).
Complex procedures
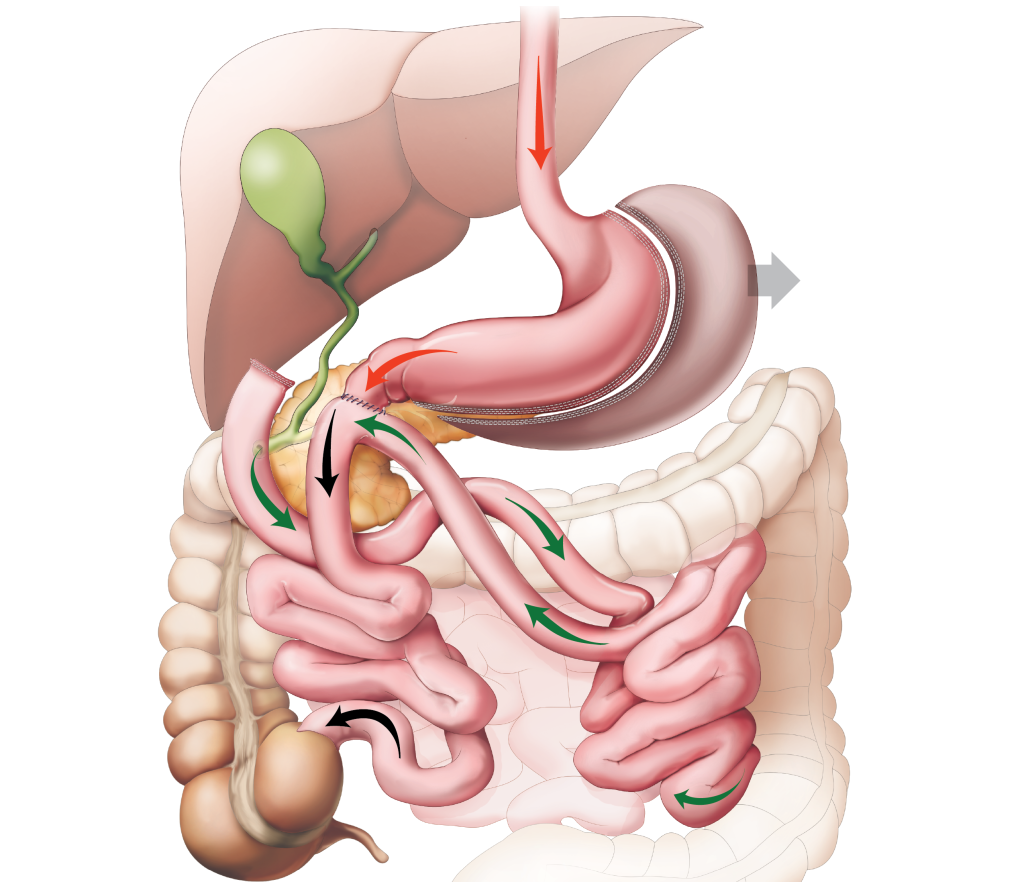
Biliopancreatic diversion with duodenal switch
Biliopancreatic diversion with duodenal switch (BPD-DS) is a surgical procedure that combines the sleeve gastrectomy with a malabsorption procedure. The biliopancreatic limb is disconnected from the food passage and reconnected to the alimentary limb at a later stage, creating a short shared resorption limb (common channel). This surgical procedure is employed as a contingency measure in instances where insufficient weight loss has been achieved following a sleeve gastrectomy, and where severe malabsorption necessitates lifelong postoperative follow-up.
Surgical procedures not establised in Switzerland
In accordance with the SMOB guidelines, surgical procedures that have not yet been established are classified as ‘in evaluation’. These procedures may only be carried out as prospective studies with a study protocol and the approval of an ethics committee.
One-anastomosis gastric bypass
The one-anastomosis gastric bypass (OAGB), also known as the omega loop bypass or, misleadingly, as a mini bypass, has gained popularity outside Switzerland. The gastric pouch is formed on the small curvature side in a similar way to the RYGB, but it is significantly longer and extends into the antrum on the small curvature side. The anastomosis is performed with a small intestinal loop in an omega formation, 150-200 cm aborally from the duodenojejunal flexure (Treitz’s flexure). Given the similarities between this procedure and the Billroth II reconstruction with an omega loop, which has been linked to an increased incidence of bile and intestinal reflux, anastomotic ulceration and anastomotic carcinoma, this procedure is only used with caution and in the context of clinical studies.
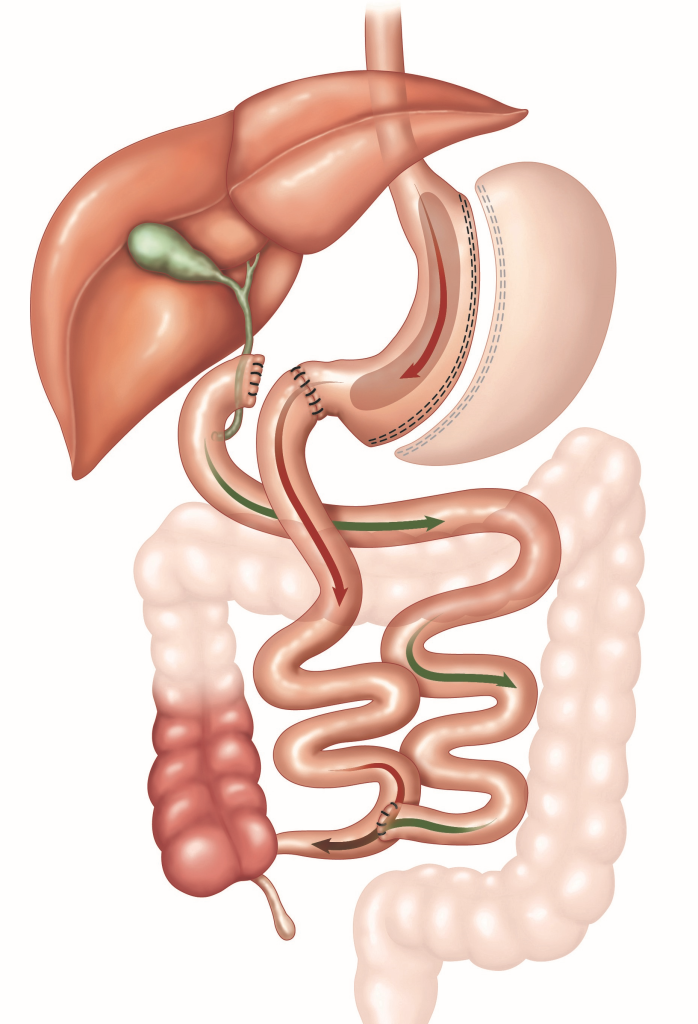
Single-anastomosis duodeno-ileal bypass with sleeve gastrectomy
The single-anastomosis duodeno-ileal bypass combines the omega formation of the small intestinal loop with the sleeve gastrectomy procedure, using only one anastomosis. This is achieved by combining the OAGB procedure with the stomach reduction (sleeve gastrectomy) and postpyloric anastomosis with the small intestine from the BPD-DS procedure. The common channel is significantly longer than in the BPD-DS procedure, at 250-300 cm. This procedure is employed when weight reduction achieved through sleeve gastrectomy is not sufficient, although reliable long-term data are still lacking.